In the super, amazing, epic news that’s actually epic column, I’m cancer-free! To say I feel thankful and grateful would be an understatement. After the doctor left the examination room, I put on my clothes and cried many happy tears.
It’s interesting that as elated as I am, I’m not in a celebratory mood. That might stem from the fact that I don’t look in the mirror and like what I see post-chemotherapy. Or, and more likely, I know – with 99% certainty – that my journey isn’t over.
If I take the doctor’s news and do nothing medically, I have a 30% chance of my cancer returning within four years. Typically, when cancer returns that quickly, it spreads beyond the area of original diagnosis. After those four years, I’d have a higher chance than the average woman of having breast cancer again. The genetics specialist believes that my mom and I have a gene that has yet to be discovered. (There is much talk of a Breast Cancer Gene, but there isn’t just one single gene that causes breast cancer.) And, I’ll need more biopsies based on the fact that I have fibrocystic breasts and many abnormal calcifications. In the past 12 years, I’ve had 13 biopsies. Eight of those were in the past four years.
When my breast surgeon recommended a lumpectomy over a mastectomy after my diagnosis, there was the assumption that I could tolerate hormonal medications after treatment. As it turns out, I can’t.
So, here I am…cancer-free…going to consultations about mastectomies and reconstruction. Tears of sadness and fear have replaced my happy tears.
Things I learned after meeting with the reconstructive surgeon:
1. 70% of women who get mastectomies with immediate reconstruction end up going in for a second corrective surgery. Out of the remaining 30%, the majority of women override their doctors’ recommendations to have a second surgery, instead choosing to live with noticeably disproportionate breasts.
2. The surgeon wouldn’t recommend me getting immediate reconstruction for several reasons:
a. I’ve had four lumpectomies over the years on my right breast alone. Scars impede blood flow to the skin. Immediate reconstruction would stretch the weak skin and jeopardize blood flood throughout.
b. I couldn’t get implants larger than a ‘C’ cup because the skin wouldn't be strong enough to support more than that. I haven’t been a ‘C’ cup since I was a teenager, and given my current size, I wouldn’t feel comfortable with that.
c. There would be an increased risk of infection for any patient, especially those with other health issues like me.
3. I will need more surgeries and the process will take much longer than expected. The general timeline is as follows:
a. Mastectomies – leave from the hospital with drains that I need to empty and clean myself and keep in place for two weeks. [Insert wincing expression here.]
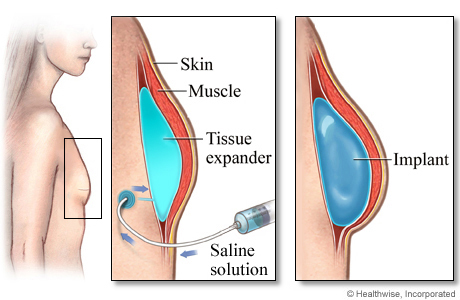
b. Expanders – I will have expanders put inside my breasts that will help stretch the skin out to my desired size. Each week, I will go into the surgeon’s office, and she will inject saline into each breast to expand them. I will be awake for this. [Insert more wincing expressions here.] She estimates that it will take four-six weeks for this process. I'm larger than a DD now, but I feel like I'll be saying, "when," by that point.
c. Wait a minimum of four to six weeks for everything to settle.
d. Have another surgery to put the permanent implants inside.
e. And, once the scars have healed (in a relative sense), have surgery or an appointment with a tattoo artist to have nipples put on.
Because of my teaching responsibilities, I won’t be getting the initial surgery until May or June, and I won’t be getting the implants put in until December. The psychic saw more surgeries in my future, but said to view them as rebuilding and strengthening. I like that in theory, but I'm going to need some time to wrap my head around that.
I’ve said before that being cancer-free doesn’t mean being done with cancer. Last week exemplified that. The thought of the expanders evokes a visceral response from me. The thought of losing my big naturals saddens me. The thought of really being done with this in a year calms me. And, when those buoyant DDs are inside me, I’ll sigh with a fair amount of relief that I have only a 5% chance of getting breast cancer in the left breast and a 12% chance in the right breast…for the rest of my life.