Twelve years ago this week, I wrote my first blog post. The topics I’ve written about have changed as my life did – from my dating debacles to sexual health to cancer to parenthood to diversity in education. And, today, I’m shifting gears again to write about something that I almost avoided posting about:
Menopause.
I gave a speed talk on menopause at my 25th college reunion. I’ve written about being thrown into medical menopause after chemotherapy. But, I haven’t been that public on my rather public social media platforms about menopause and post-menopause. I felt stuck between Sex and the City and Golden Girls, and it was neither sexy nor golden.
So, why am I writing this now? Most importantly, I want my friends who feel as though they’re going through all these confusing changes alone to know that they aren’t. For people with loved ones in menopause, I hope they can learn something, too. It also is part of who I am to talk about that which is uncomfortable. Lastly, I write this as someone who is now post-menopausal with a greater knowledge base and appreciation for what my body has endured.
What does it mean to be in menopause?
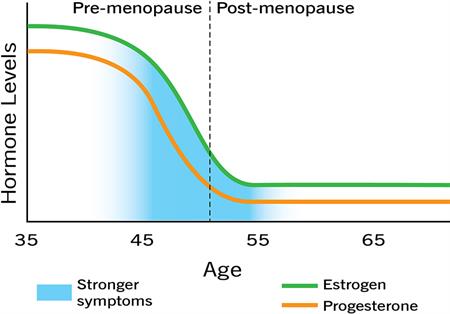
“In menopause” is a catch-all term that makes the experience seem like more of a discrete event than it is. There are three stages of menopause: 1) perimenopause; 2) menopause; and 3) post-menopause. Today, I’ll be focusing on perimenopause (also known as pre-menopause or the transition to menopause).
Am I in perimenopause?
On average, perimenopause starts at 47, and menopause at 51. But, for some, perimenopause can start in their* 30s, and for others, it can start in their 50s. It’s worth asking older relatives who have been through menopause as to their age and experience with it.
The most obvious signs that you’ve started perimenopause are:
- Period Changes:
- Your periods can become irregular in terms of the amount of bleeding, frequency, and duration. Remember when you were a teenager and you never knew when your period would come, how long it would last, and what clothes or bedding would get stained in the process? Yes, perimenopause can be reminiscent of that. Be prepared!
- During this stage, your ovaries are producing less estrogen and fewer eggs, but you can still get pregnant.
- For 25-30% of people in perimenopause, periods can be significantly heavier. You might wish to speak with your GYN about options.
- If you are using a form of birth control with hormones such as the IUD or the pill, or have had a hysterectomy, you may not notice a change in your periods.
- Menopausal symptoms
- During perimenopause, your body is adjusting to a decrease in estrogen. This may cause a range of symptoms, including sleep disturbances, mood changes, headaches, joint pain, slowed metabolism, bladder issues, digestive problems, and vaginal pain. Saska Graville for MPowered cites 34(!) possible menopause symptoms.
- 85% of those in menopause experience hot flashes. During a hot flash, your skin temperature can increase by five-seven degrees. (Hot flashes do not change your core body temperature, though. If you’re wondering whether it’s a fever or a hot flash, check your temperature with an oral thermometer, not a temperature scanner.) On average, hot flashes last for four minutes.
- Some may get many of these symptoms, and some very few. Hormonal birth control and hormonal replacement therapy [HRT] may reduce the severity of these symptoms. Talk with your GYN or internist as to whether you may benefit from these options. Also make sure to factor in your risk of breast cancer, heart disease, and osteoporosis into your conversations about HRT.
- If you don’t feel comfortable talking with your doctor about these topics, my old post about talking to your doctor about sex can be adapted for menopause.
- Blood tests — Blood tests can rule out other health issues with similar symptoms like thyroid problems, while checking your hormone levels. Since hormones fluctuate during perimenopause, you may need more than one blood test to look at your follicle-stimulating hormone levels (FSH).
How long will perimenopause last?
On average, this stage lasts four years, but again, every body is different. For some, symptoms are minimal and last only a few months. Others experience a multitude of symptoms with perimenopause lasting up to 10 years.
In my next post, I’ll explore menopause and post-menopause and then shift back to anti-racist resources. Until then, please comment and post.
Be well xoxo
* Since 2008, the majority of my posts were written as though everyone with a vagina identified as female. I know better now and am trying to approach this post correctly using gender-inclusive language.
** Disclaimer: Although I wear many hats, I’m not a doctor nor do I play one on TV. This post is not a substitute for medical advice. Hyperlinks are plentiful in this post to help steer you toward additional information from reliable medical sites.
Thank you, Stef!
What a fantastic idea for our class (and others)…we are roughly going through the same things in this regard and I really appreciate the material.
Thank you so much for commenting! I’m so glad you found the post helpful. Happy New Year :)!
Great post, Stef! I had a total hysterectomy in 2001, so went immediately into menopause. My doctor recommend a natural estrogen replacement, so I literally started it in the recovery room. Because of that, I didn’t experience a lot of the symptoms many people do. No hot flashes, or other side effects. About 10 years ago I decided to stop taking the estrogen, and again I was fortunate to not have a lot of side effects. My overall body temperature increased, so while some people need a heavy coat, I can often get by with a lighter coat or jacket.
My decision to have the surgery was prompted by a large fibroid tumor growing in my uterus that caused me to have very heavy flow during my periods. It was so annoying that I asked my ob-gyn if I could just have everything removed! He recommended that I have my ovaries removed as a prophylactic measure. I never regretted it, as it was the best decision to make at the time!
Thank you for sharing your story, Beth! I’m so glad that it was the right call for you and that you experienced minimal symptoms. From what I’ve read and heard, symptoms following a hysterectomy and bilateral oophorectomy vary, too. I do think the ability to take HRT helps. Again, so glad this combination worked for you xoxo
Thanks Stef!! Class of ‘94 is thrilled to have you guide us through this often-misunderstood chapter of our lives.
Truly thankful we all have each other to learn and grow! And, our class definitely inspired me to keep up with my research and write/speak more about this. Happy New Year, Amy xoxo