As I mentioned in my Menopause post, once your periods cease and you are postmenopausal, you are at a higher risk of several health issues, including:
- Heart Disease
- Osteoporosis
- Bladder Issues
- Vaginal/Pelvic Floor Problems; and
- Weight Gain.
A higher risk is subjective, and not everyone experiencing menopause will have any — let alone all — of the above issues. Today, let’s explore heart disease and menopause.
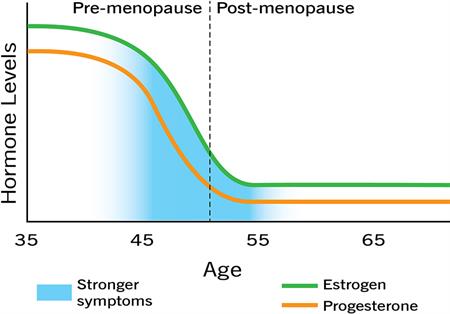
Heart disease is the leading cause of death in adult females. According to the American Heart Association, a decline in estrogen levels, a rise in blood pressure, and a rise in the “bad” cholesterol during menopause may contribute to the rise in heart attacks among cisgender women 10 years after menopause. (Note that available research and statistics frame heart disease and cardiovascular risk through a gender-binary lens.)
You can evaluate your risk level for heart disease via the CDC website here. The CDC site notes that “about half of all Americans (47%) have at least 1 of 3 key risk factors for heart disease: high blood pressure, high cholesterol, and smoking.”
During your annual physical with your primary-care physician, you can have your blood pressure checked, confirm via a blood test that cholesterol is in a normal range, and discuss your family health history and your risk for heart disease. This appointment also serves as an opportunity to evaluate whether you should see a preventative cardiologist.
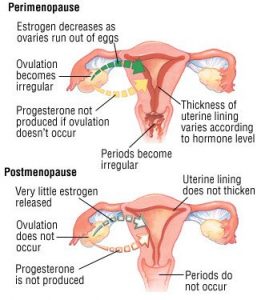
Being in some stage within menopause also should be part of this conversation. As the Mayo Clinic describes, hormonal changes such as menopause and hormone-replacement therapy make some people more sensitive to salt and/or cause weight gain. Both of these things may increase your blood pressure, and that, in turn, is one of the key risk factors for heart disease.
This weekend is the American Heart Association Walk in Washington, DC. The organization has been at the forefront of the fight against stroke and heart disease for over 90 years. I encourage you and your family to talk about heart disease risks, learn more, and share critical information with others. If you’re in a position to volunteer or donate, there are so many ways to help through the American Heart Association and local organizations and hospitals.
Note: I continue to be neither a doctor nor do I play one on TV so please discuss your health history and risks with your doctors. xoxo